Interpreting body fat percentage
Excess body fat is associated with certain health outcomes like cardiovascular disease risk and all-cause mortality1. It may also have implications for sport performance. For these reasons, it is often valuable to know and track this over time. However, it is unfortunately, also one of the trickier metrics to measure accurately.

The most direct method for assessing body fat percentage is through cadaver dissection. While it may be accurate, it’s not practical (for obvious reasons). There are several indirect methods that predict body fat percentage based on different models (Fig. 1)2. These use different techniques (X-rays, electric currents, skinfold thickness, fluid displacement, etc) to predict body composition according to two, three, and four component models. The models effectively divide the body into certain components. For example, the two-compartment model uses the thickness of skinfolds at certain sites and divides the body into either fat free mass or fat mass. Fat mass includes all types of fat tissue (e.g., adipose and visceral) where fat free mass includes muscles, bones, organs, water, etc.
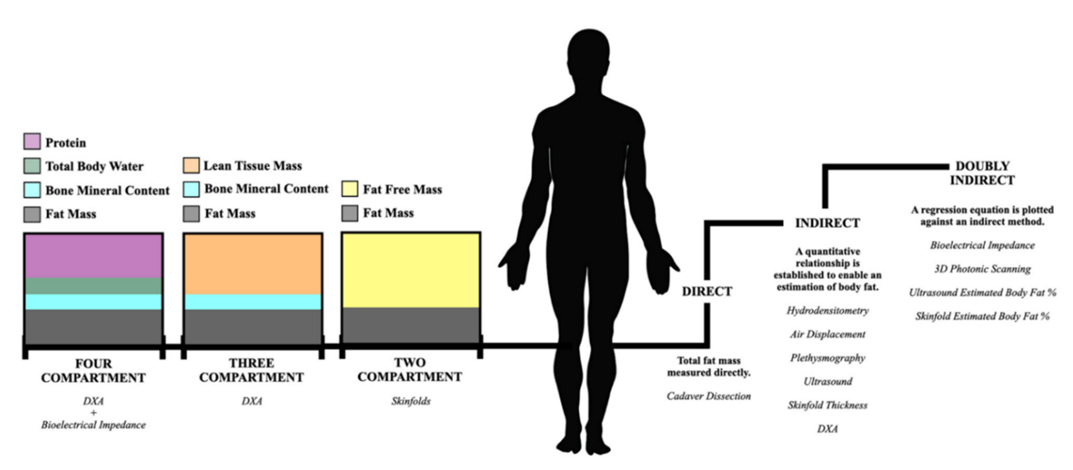
Figure 1: Summary of body fat percentage measurement methods taken from Kasper et al., 20212.
To date, the Dual-energy X-ray Absorptiometry (DXA) method is considered the gold standard for measuring body fat percentage. While highly accurate, it is extremely expensive and often inaccessible. Popular alternatives include bioelectrical impedance analysis or BIA (e.g., Technogym CheckUp & Inbody) and 3D body scanners (e.g., Styku & Human Solutions).
Recently, Thomas and colleagues published a good resource that reviewed these methods and discussed the advantages and disadvantages of each method3.
Body scanners may be acceptably accurate although depending on the device, can overestimate body fat percentage between 2 and 8% compared to DXA. They also tend to show wide limits of agreement (i.e., high variability between individuals). This means it may be more accurate for some but less for others. While accuracy may vary, reliability tends to be good when test is done appropriately (e.g., form fitting clothing). This means it can be used to track changes over time.
Bioelectrical Impedance Analysis (BIA) shows extremely limited agreement on an individual level when compared with DXA. It tends to underestimate fat mass and overestimate fat free mass – underestimating body fat %. Overall, accuracy is considered limited and varies highly between individuals. However, for certain populations there are calibrations that can be done to improve accuracy. Reliability of BIA is limited and depends largely on hydration status, previous meals and exercise.
Table 1: Summary of methods used to measure body fat percentage3
|
Method |
Description |
Accuracy |
Reliability |
|
DXA |
Uses high and low energy X-ray beams to determine body composition. This is based on the differing elemental make up of tissues absorbs X-rays. |
Good.
|
Excellent.
Dependent on prior food intake, hydration, and exercise. |
|
BIA |
Uses (small) electrical impulses to estimate body fat percentage, based resistance of the electric current. Fat tissue is treated as “resistance” to the flow of current. |
Varied.
|
Varied.
Highly dependent on hydration status, prior exercise, meal timing. |
|
3D Body Scans |
Either measures the disturbance of light or the time it takes for the light to reflect to the sensor to produce a 3D avatar based on morphology. This is then plugged into an algorithm that predicts body composition. |
Varied. |
Excellent.
Dependent on clothing/position. |
Overall, body composition assessment is clouded with error and variability. This is essential to understand as is provides useful context for the interpretation of body composition results. Typically, it isn’t appropriate to compare results from different devices. While self-measurement is convenient, often a visit to a professional help eliminate sources of error through the adherence to standard protocols.
To help you navigate the path of monitoring body composition, we’ve provided some practical steps you can follow to ensure accurate and reliable data.
Practical Steps for Monitoring Body Composition
- Pick an accurate & reliable device/method.
- Use the same device/method.
- Control for confounding variables
- Time of day, clothing, exercise, hydration, etc.
- Interpret results with device &
- Find the correct reference data for that method (e.g., Table 2)
- If concerned/confused, discuss with a health professional.
Table 2: Adult body fat percentage classification as assessed by DXA4.
|
|
Women |
Men |
|
Essential fat |
<15% |
<10% |
|
Athlete |
15-19% |
10-14% |
|
Fitness |
20-24% |
15-19% |
|
Acceptable |
25-29% |
20-24% |
|
Pre-obesity |
30-34% |
25-29% |
|
Obesity |
>35% |
>30% |
Summary and Reality Check:
Body fat percentage is an important health metric, but measuring it accurately is challenging. DXA is the gold standard for accuracy but is costly and less accessible, while BIA and 3D body scanners like Styku are more convenient but less reliable—BIA’s results vary with hydration and other factors, and 3D scanners can overestimate fat. For best results, use the same method each time, control for variables like time and hydration, and consult a professional for interpretation, as comparing results across different devices is not recommended.
References
1. Myint P, Kwok C, Luben R, Wareham N, Heart KK, 2014 undefined. Body fat percentage, body mass index and waist-to-hip ratio as predictors of mortality and cardiovascular disease. heart.bmj.com [Internet]. [cited 2024 Apr 19]; Available from: https://heart.bmj.com/content/100/20/1613.short?
- Kasper AM, Langan‐evans C, Hudson JF, Brownlee TE, Harper LD, Naughton RJ, et al. Come back skinfolds, all is forgiven: A narrative review of the efficacy of common body composition methods in applied sports practice. Vol. 13, Nutrients. MDPI AG; 2021.
- Thomas DM, Crofford I, Scudder J, Oletti B, Deb A, Heymsfield SB. Updates on Methods for Body Composition Analysis: Implications for Clinical Practice. Vol. 14, Current Obesity Reports. Springer; 2025.
- Burridge K, Christensen SM, Golden A, Ingersoll AB, Tondt J, Bays HE. Obesity history, physical exam, laboratory, body composition, and energy expenditure: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022. Obesity Pillars. 2022;1(December 2021):100007.
Fit4Living with SSISA
Think Fit4Living. Think The Sports Science Institute of South Africa.



